Metformin
Overview
Description
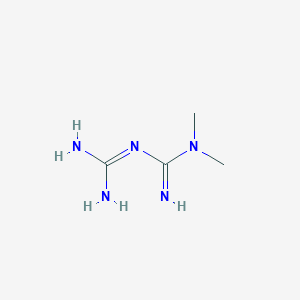
Metformin, a biguanide derivative, is a first-line oral antidiabetic agent prescribed globally for type 2 diabetes mellitus (T2DM). It is included in the WHO Model List of Essential Medicines due to its efficacy, safety, and affordability . Its primary mechanisms include:
- Suppression of hepatic glucose production via AMP-activated protein kinase (AMPK) activation .
- Enhancing peripheral glucose uptake and improving insulin sensitivity .
- Gut-mediated effects, such as stimulating GLP-1 secretion and altering bile acid metabolism .
Approved indications include T2DM, gestational diabetes (in some regions), and polycystic ovary syndrome (PCOS). Off-label uses span prediabetes, antipsychotic-induced weight gain, and cancer prevention . The Diabetes Prevention Program (DPP) trial demonstrated this compound reduces T2DM incidence by 31% compared to placebo, though lifestyle intervention was superior (58% risk reduction) .
Preparation Methods
Synthetic Routes and Reaction Conditions: Metformin is synthesized through the reaction of dimethylamine hydrochloride with dicyandiamide. The reaction is typically carried out under heating conditions, often using microwave irradiation at temperatures ranging from 100 to 160°C .
Industrial Production Methods: In industrial settings, this compound hydrochloride is produced by heating raw materials such as dicyandiamide and dimethylamine hydrochloride. The reaction is conducted in a controlled environment to ensure high yield and purity of the final product .
Chemical Reactions Analysis
Reaction with α-Dicarbonyl Compounds
Metformin reacts with reactive glycation agents like methylglyoxal (MGO) and glyoxal (GO), forming guanidine-dicarbonyl adducts :
These reactions inhibit advanced glycation end product (AGE) formation, suggesting a therapeutic role in mitigating diabetic complications .
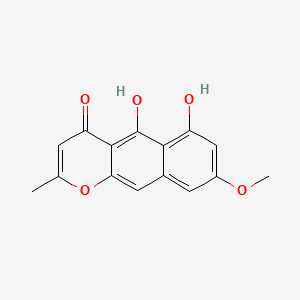
Formation of 1,3,5-Triazine Derivatives
This compound undergoes cyclization reactions to form triazine-based compounds with potential pharmacological applications :
| Reactants | Conditions | Product | Yield |
|---|---|---|---|
| This compound + Methyl bromoacetate-magnolol adduct | NaOCH₃, MeOH, 65°C, 6 hrs | 1,3,5-Triazine derivative | 86% |
This reaction leverages this compound’s biguanide structure to create heterocyclic compounds, enhancing its utility in drug development .
Interaction with Mitochondrial Complex I
While not a classical chemical reaction, this compound’s inhibition of mitochondrial complex I alters cellular redox states:
| Parameter | Effect Observed | Concentration Range |
|---|---|---|
| AMP:ATP ratio | ↑ 2–3 fold | 50–100 μM (clinical) |
| NADH:NAD⁺ ratio | ↑ 30–40% | 1–10 mM (in vitro) |
This redox modulation underpins its AMP-activated protein kinase (AMPK)-independent antidiabetic effects .
Stability and Degradation
This compound hydrochloride is stable under standard storage conditions but degrades under extreme pH or heat:
| Condition | Degradation Product | Method of Analysis |
|---|---|---|
| pH < 2 or pH > 10 | Biguanide breakdown | HPLC-MS |
| 100°C, 48 hrs | Cyanoguanidine derivatives | NMR, LC-MS |
Stability studies confirm its robustness in pharmaceutical formulations within pH 3–7 .
Analytical Characterization
Key spectral data for this compound identification:
| Technique | Key Peaks/Features | Reference |
|---|---|---|
| ¹H-NMR (D₂O) | δ 2.86 (s, 6H, N-CH₃) | |
| LC-MS (ESI+) | m/z 130.1 [M+H]⁺ | |
| FT-IR | 1565 cm⁻¹ (C=N stretch) |
Scientific Research Applications
Metformin in Diabetes Management
Mechanism of Action
this compound primarily reduces blood glucose levels by inhibiting gluconeogenesis in the liver and improving insulin sensitivity in peripheral tissues. It also decreases intestinal glucose absorption and reduces free fatty acid release from adipose tissue .
Clinical Efficacy
- Type 2 Diabetes : this compound remains the first-line treatment for T2DM, with significant evidence supporting its efficacy in lowering HbA1c levels and reducing the risk of diabetes-related complications .
- Prediabetes : The Diabetes Prevention Program (DPP) demonstrated that this compound effectively delays the progression from prediabetes to diabetes .
Oncological Applications
This compound has emerged as a promising agent in cancer treatment due to its potential anti-tumor effects.
Cancer Types and Findings
- Breast Cancer : Studies indicate that this compound sensitizes breast cancer cells to chemotherapy by targeting cancer stem cells (CSCs) and improving the hypoxic microenvironment .
- Ovarian Cancer : A phase II trial showed that this compound improved progression-free survival (PFS) and overall survival (OS) in nondiabetic patients with advanced ovarian cancer, suggesting its role as a chemosensitizer .
- Colorectal Cancer : Evidence suggests that this compound may reduce the risk of colorectal cancer incidence and mortality among diabetic patients .
Cardiovascular Benefits
This compound has been associated with cardiovascular benefits beyond its glucose-lowering effects.
- Heart Failure : Meta-analyses have shown that this compound reduces all-cause mortality in patients with heart failure and T2DM .
- Anti-inflammatory Effects : this compound exhibits anti-inflammatory properties that may contribute to cardiovascular protection .
Neuroprotective Properties
Recent studies have explored this compound's potential in neurodegenerative diseases.
- Alzheimer's Disease : this compound is being investigated for its neuroprotective effects and ability to improve cognitive function in patients with mild cognitive impairment .
- Duchenne Muscular Dystrophy : Research indicates that this compound may slow disease progression in Duchenne muscular dystrophy patients .
Infectious Disease Applications
This compound has shown promise in treating various infectious diseases.
- COVID-19 : A study found that this compound significantly reduced viral load and hospitalization rates among COVID-19 patients, suggesting its potential as an adjunct therapy .
- Tuberculosis : Preliminary data indicate possible benefits of this compound in tuberculosis treatment, although further studies are needed to confirm these findings .
Summary Table of this compound Applications
| Application Area | Specific Use Cases | Key Findings |
|---|---|---|
| Diabetes Management | T2DM, Prediabetes | First-line treatment; delays progression from prediabetes to diabetes |
| Oncology | Breast, Ovarian, Colorectal Cancer | Sensitizes tumors to chemotherapy; improves survival rates |
| Cardiovascular Health | Heart Failure | Reduces all-cause mortality; exhibits anti-inflammatory effects |
| Neuroprotection | Alzheimer's Disease, Duchenne Muscular Dystrophy | Improves cognitive function; slows disease progression |
| Infectious Diseases | COVID-19, Tuberculosis | Reduces viral load; potential adjunct therapy for tuberculosis |
Mechanism of Action
Metformin exerts its effects through several mechanisms:
Decreasing Hepatic Glucose Production: this compound inhibits gluconeogenesis in the liver, reducing glucose production.
Increasing Insulin Sensitivity: It enhances the sensitivity of peripheral tissues to insulin, promoting glucose uptake.
Modulating Gut Microbiota: this compound alters the composition of gut microbiota, which may contribute to its glucose-lowering effects.
Molecular Targets and Pathways: this compound primarily targets the liver and gastrointestinal tract.
Comparison with Similar Compounds
Comparison with Other Antidiabetic Agents
Thiazolidinediones (TZDs: Pioglitazone, Rosiglitazone)
TZDs improve insulin sensitivity in adipose tissue and skeletal muscle but are associated with weight gain and cardiovascular risks, limiting their use in heart failure patients. This compound is preferred for obesity-related T2DM due to weight-neutral effects .
Sulfonylureas (Glimepiride, Glyburide)
Sulfonylureas achieve similar glycemic control but pose higher hypoglycemia risk, especially in older adults. This compound is safer in non-renally impaired patients .
DPP-4 Inhibitors (Sitagliptin, Saxagliptin)
| Parameter | This compound | DPP-4 Inhibitors |
|---|---|---|
| Mechanism | AMPK activation; gut-mediated effects | Incretin enhancement (GLP-1 prolongation) |
| HbA1c Reduction | ~1.0–1.5% | ~0.5–0.8% |
| Weight Effects | Neutral or modest loss | Neutral |
| Cost | Low | High |
| Cardiovascular Safety | Neutral | Saxagliptin linked to heart failure risk |
DPP-4 inhibitors are weight-neutral but less potent than this compound. They are often used as add-ons to this compound but lack cost-effectiveness as monotherapy .
Comparison of this compound Formulations
XR formulations reduce GI adverse events (e.g., diarrhea, nausea) by 34% compared to IR, with comparable efficacy. However, XR is costlier, limiting use in resource-constrained settings .
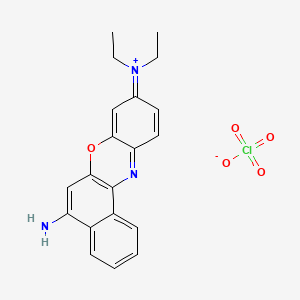
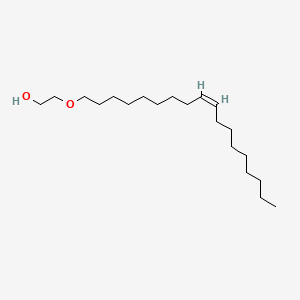
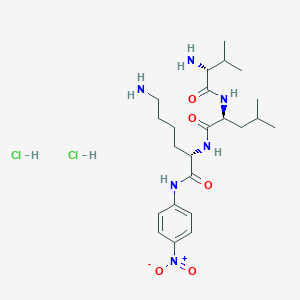
Comparison with Transition Metal Complexes
This compound complexes with metals (e.g., Nd(III), La(III)) aim to enhance bioavailability or target-specific effects. For example:
- This compound alone in diabetic rats .
- Chromium(III)-Metformin : Improved insulin sensitivity in preclinical studies but lacks clinical validation .
Biological Activity
Metformin, a widely used medication for type 2 diabetes, exhibits a range of biological activities that extend beyond glucose regulation. Its mechanisms of action are complex and involve multiple pathways, including the activation of AMP-activated protein kinase (AMPK), modulation of mitochondrial function, and alterations in gut microbiota. This article delves into the biological activity of this compound, supported by recent research findings, case studies, and data tables.
AMPK Activation
this compound primarily activates AMPK, a critical energy sensor in cells. This activation occurs through various mechanisms:
- Mitochondrial Inhibition : this compound inhibits complex I of the mitochondrial electron transport chain, leading to decreased ATP production and increased AMP levels. The elevated AMP activates AMPK, which subsequently reduces hepatic gluconeogenesis and promotes glucose uptake in peripheral tissues .
- Redox State Modulation : Recent studies indicate that this compound can alter the cellular redox balance, inhibiting glycerol-3-phosphate dehydrogenase 2 (GPD2) at clinically relevant concentrations (50-100 μM). This inhibition contributes to reduced gluconeogenesis in a substrate-selective manner .
Gut Microbiota Interaction
this compound also influences gut microbiota composition, which may play a role in its glucose-lowering effects. It has been shown to increase the production of glucagon-like peptide-1 (GLP-1), enhancing insulin secretion and improving glucose homeostasis .
Biological Activities Beyond Diabetes
Recent research has uncovered additional biological activities of this compound that suggest potential therapeutic applications:
- Anti-Aging Effects : Studies have indicated that this compound may extend lifespan in model organisms like C. elegans through AMPK activation pathways .
- Antimicrobial Properties : this compound has demonstrated dose-dependent antimicrobial activity against various microorganisms, indicating its potential role in infectious disease management .
- Cancer Prevention : Epidemiological studies suggest that this compound use is associated with a reduced risk of certain cancers, likely due to its effects on insulin sensitivity and inflammation .
Case Studies
Several case studies highlight the diverse effects of this compound:
- Vitamin B12 Deficiency : A clinical audit found a significant prevalence of low vitamin B12 status among patients receiving this compound therapy, suggesting the need for monitoring and supplementation in long-term users .
- Drug Interactions : Research indicates that certain drugs can affect the pharmacokinetics of this compound. For instance, mavorixafor was reported to reduce the effectiveness of this compound by decreasing its maximum serum concentration (Cmax) and area under the curve (AUC) .
Research Findings
Recent studies have provided insights into the multifaceted actions of this compound:
Q & A
Basic Research Questions
Q. What are the primary molecular mechanisms through which metformin exerts its antidiabetic and potential anticancer effects?
- Category : Basic Research (Mechanistic Insights)
- Answer : this compound primarily activates AMP-activated protein kinase (AMPK), a cellular energy sensor that inhibits hepatic gluconeogenesis and enhances glucose uptake in skeletal muscle . In cancer research, AMPK activation suppresses mTOR signaling, inhibiting tumor cell proliferation. Preclinical studies further suggest this compound reduces hyperinsulinemia, a factor linked to cancer progression . Methodologically, researchers validate AMPK involvement via siRNA knockdowns or AMPK-null cell models, coupled with metabolomic profiling to assess downstream effects.
Q. How do researchers standardize therapeutic this compound concentrations in pharmacokinetic studies?
- Category : Basic Research (Pharmacokinetics)
- Answer : Therapeutic plasma concentrations typically range between 1–2 µg/mL, but variability exists due to renal function, dosing, and patient demographics. Analytical methods include high-performance liquid chromatography (HPLC) with UV detection and liquid chromatography-tandem mass spectrometry (LC-MS/MS) for enhanced specificity . Researchers must calibrate assays using validated reference standards (e.g., European Pharmacopoeia guidelines) and account for matrix effects in biological samples .
Q. What methodologies are employed to assess this compound’s safety in gestational diabetes (GD) and lactation?
- Category : Basic Research (Clinical Safety)
- Answer : Cohort studies track maternal-fetal outcomes, including neonatal hypoglycemia and small-for-gestational-age (SGA) incidence, using longitudinal anthropometric and metabolic data . Pharmacokinetic studies in pregnant women compare this compound bioavailability and clearance to non-pregnant cohorts, adjusting for pregnancy-induced changes in renal function . Ethical considerations require stratification by trimester and exclusion of high-risk comorbidities (e.g., preeclampsia).
Advanced Research Questions
Q. How can residual confounding be mitigated in observational studies investigating this compound’s anticancer effects?
- Category : Advanced Research (Epidemiological Design)
- Answer : Propensity score matching balances covariates like age, BMI, and diabetes severity between this compound users and non-users . Sensitivity analyses test robustness against unmeasured confounders (e.g., smoking, genetic risk). Recent protocols recommend triangulating observational data with RCTs and Mendelian randomization to infer causality . For example, Evans et al. (2005) adjusted for smoking and socioeconomic status in their cancer risk analysis .
Q. What experimental designs are optimal for evaluating this compound’s efficacy as an adjunct therapy in oncology?
- Category : Advanced Research (Clinical Trials)
- Answer : Phase II neoadjuvant trials (e.g., Jiralerspong et al., 2009) measure pathologic complete response (pCR) rates in breast cancer patients receiving this compound with chemotherapy. Key considerations include stratification by tumor subtype (e.g., triple-negative) and this compound dosing (e.g., 850 mg BID) . For survival endpoints, Cox regression models adjust for diabetes status and comorbidities, as in Sadeghi et al. (2012)’s pancreatic cancer study .
Q. How can contradictory findings on this compound’s association with cancer survival be resolved?
- Category : Advanced Research (Data Analysis)
- Answer : Meta-analyses (e.g., NSCLC studies ) subgroup by cancer stage, this compound duration, and glycemic control. For example, advanced NSCLC shows stronger survival benefits than localized disease . Discrepancies between observational studies and RCTs may arise from immortal time bias, addressed via time-dependent Cox models . Researchers should also harmonize endpoints (e.g., overall survival vs. progression-free survival) across datasets.
Q. What strategies optimize this compound quantification in complex biological matrices for pharmacokinetic studies?
- Category : Advanced Research (Analytical Chemistry)
- Answer : Solid-phase extraction (SPE) prior to LC-MS/MS improves recovery from plasma/urine . Cation-exchange chromatography separates this compound from cationic interferents (e.g., creatinine) . Method validation follows ICH guidelines, assessing linearity (1–10 µg/mL), precision (CV <15%), and stability under storage conditions .
Q. How do researchers design dose-escalation studies for this compound in non-diabetic populations (e.g., cancer prevention)?
- Category : Advanced Research (Translational Pharmacology)
- Answer : Phase I trials use adaptive designs to identify maximum tolerated doses (MTD), monitoring lactate levels to avoid acidosis. Pharmacodynamic endpoints include AMPK activation in peripheral blood mononuclear cells (PBMCs) . For preclinical models, xenograft studies correlate plasma this compound levels with tumor growth inhibition, using species-specific pharmacokinetic scaling .
Q. Methodological Considerations
- Data Contradictions : Address heterogeneity via individual participant data (IPD) meta-analysis, as in the Cochrane protocol for endometrial hyperplasia .
- Green Chemistry : Prioritize eco-friendly analytical methods (e.g., reduced solvent use in HPLC) per the 12 Principles of Green Analytical Chemistry .
- Ethical Compliance : In gestational studies, obtain informed consent for long-term offspring follow-up to assess developmental outcomes .
Properties
IUPAC Name |
3-(diaminomethylidene)-1,1-dimethylguanidine | |
|---|---|---|
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI |
InChI=1S/C4H11N5/c1-9(2)4(7)8-3(5)6/h1-2H3,(H5,5,6,7,8) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI Key |
XZWYZXLIPXDOLR-UHFFFAOYSA-N | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Canonical SMILES |
CN(C)C(=N)N=C(N)N | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Formula |
C4H11N5 | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
DSSTOX Substance ID |
DTXSID2023270 | |
| Record name | Metformin | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID2023270 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
Molecular Weight |
129.16 g/mol | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Physical Description |
Solid | |
| Record name | 1,1-Dimethylbiguanide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0001921 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Boiling Point |
224.1ºC at 760 mmHg | |
| Record name | Metformin | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00331 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
Solubility |
Freely soluble | |
| Record name | Metformin | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00331 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
Mechanism of Action |
Metformin's mechanisms of action are unique from other classes of oral antihyperglycemic drugs. Metformin decreases blood glucose levels by decreasing hepatic glucose production (also called gluconeogenesis), decreasing the intestinal absorption of glucose, and increasing insulin sensitivity by increasing peripheral glucose uptake and utilization. It is well established that metformin inhibits mitochondrial complex I activity, and it has since been generally postulated that its potent antidiabetic effects occur through this mechanism. The above processes lead to a decrease in blood glucose, managing type II diabetes and exerting positive effects on glycemic control. After ingestion, the organic cation transporter-1 (OCT1) is responsible for the uptake of metformin into hepatocytes (liver cells). As this drug is positively charged, it accumulates in cells and in the mitochondria because of the membrane potentials across the plasma membrane as well as the mitochondrial inner membrane. Metformin inhibits mitochondrial complex I, preventing the production of mitochondrial ATP leading to increased cytoplasmic ADP:ATP and AMP:ATP ratios. These changes activate AMP-activated protein kinase (AMPK), an enzyme that plays an important role in the regulation of glucose metabolism. Aside from this mechanism, AMPK can be activated by a lysosomal mechanism involving other activators. Following this process, increases in AMP:ATP ratio also inhibit _fructose-1,6-bisphosphatase_ enzyme, resulting in the inhibition of gluconeogenesis, while also inhibiting _adenylate cyclase_ and decreasing the production of cyclic adenosine monophosphate (cAMP), a derivative of ATP used for cell signaling. Activated AMPK phosphorylates two isoforms of acetyl-CoA carboxylase enzyme, thereby inhibiting fat synthesis and leading to fat oxidation, reducing hepatic lipid stores and increasing liver sensitivity to insulin. In the intestines, metformin increases anaerobic glucose metabolism in enterocytes (intestinal cells), leading to reduced net glucose uptake and increased delivery of lactate to the liver. Recent studies have also implicated the gut as a primary site of action of metformin and suggest that the liver may not be as important for metformin action in patients with type 2 diabetes. Some of the ways metformin may play a role on the intestines is by promoting the metabolism of glucose by increasing glucagon-like peptide I (GLP-1) as well as increasing gut utilization of glucose. In addition to the above pathway, the mechanism of action of metformin may be explained by other ways, and its exact mechanism of action has been under extensive study in recent years., Metformin is widely used to treat hyperglycemia. However, metformin treatment may induce intrahepatic cholestasis and liver injury in a few patients with type II diabetes through an unknown mechanism. Here we show that metformin decreases SIRT1 protein levels in primary hepatocytes and liver. Both metformin-treated wild-type C57 mice and hepatic SIRT1-mutant mice had increased hepatic and serum bile acid levels. However, metformin failed to change systemic bile acid levels in hepatic SIRT1-mutant mice. Molecular mechanism study indicates that SIRT1 directly interacts with and deacetylates Foxa2 to inhibit its transcriptional activity on expression of genes involved in bile acids synthesis and transport. Hepatic SIRT1 mutation elevates Foxa2 acetylation levels, which promotes Foxa2 binding to and activating genes involved in bile acids metabolism, impairing hepatic and systemic bile acid homeostasis. Our data clearly suggest that hepatic SIRT1 mediates metformin effects on systemic bile acid metabolism and modulation of SIRT1 activity in liver may be an attractive approach for treatment of bile acid-related diseases such as cholestasis., Metformin is antihyperglycemic, not hypoglycemic. It does not cause insulin release from the pancreas and does not cause hypoglycemia, even in large doses. Metformin has no significant effects on the secretion of glucagon, cortisol, growth hormone or somatostatin. Metformin reduces glucose levels primarily by decreasing hepatic glucose production and by increasing insulin action in muscle and fat. ... May decrease plasma glucose by reducing the absorption of glucose from the intestine. /Salt not specified/, Metformin potentiates the effect of insulin by mechanisms not fully understood. Metformin does not stimulate pancreatic beta cells to increase secretion of insulin; insulin secretion must be present for metformin to work properly. It is postulated that metformin decreases hepatic glucose production and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. /Salt not specified/, People with Type 2 diabetes mellitus (T2DM) have reduced bone mineral density and an increased risk of fractures due to altered mesenchymal stem cell (MSC) differentiation in the bone marrow. This leads to a shift in the balance of differentiation away from bone formation (osteogenesis) in favour of fat cell development (adipogenesis). The commonly used anti-diabetic drug, metformin, activates the osteogenic transcription factor Runt-related transcription factor 2 (Runx2), which may suppress adipogenesis, leading to improved bone health. Here we investigate the involvement of the metabolic enzyme, AMP-activated protein kinase (AMPK), in these protective actions of metformin. The anti-adipogenic actions of metformin were observed in multipotent C3H10T1/2 MSCs, in which metformin exerted reciprocal control over the activities of Runx2 and the adipogenic transcription factor, PPARgamma, leading to suppression of adipogenesis. These effects appeared to be independent of AMPK activation but rather through the suppression of the mTOR/p70S6K signalling pathway. Basal AMPK and mTOR/p70S6K activity did appear to be required for adipogenesis, as demonstrated by the use of the AMPK inhibitor, compound C. This observation was further supported by using AMPK knockout mouse embryo fibroblasts (MEFs) where adipogenesis, as assessed by reduced lipid accumulation and expression of the adipogeneic transcription factor, C/EBPbeta, was found to display an absolute requirement for AMPK. Further activation of AMPK in wild type MEFS, with either metformin or the AMPK-specific activator, A769662, was also associated with suppression of adipogenesis. It appears, therefore, that basal AMPK activity is required for adipogenesis and that metformin can inhibit adipogenesis through AMPK-dependent or -independent mechanisms, depending on the cellular context. | |
| Record name | Metformin | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00331 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | METFORMIN | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/7080 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
CAS No. |
657-24-9, 1115-70-4 | |
| Record name | Metformin | |
| Source | CAS Common Chemistry | |
| URL | https://commonchemistry.cas.org/detail?cas_rn=657-24-9 | |
| Description | CAS Common Chemistry is an open community resource for accessing chemical information. Nearly 500,000 chemical substances from CAS REGISTRY cover areas of community interest, including common and frequently regulated chemicals, and those relevant to high school and undergraduate chemistry classes. This chemical information, curated by our expert scientists, is provided in alignment with our mission as a division of the American Chemical Society. | |
| Explanation | The data from CAS Common Chemistry is provided under a CC-BY-NC 4.0 license, unless otherwise stated. | |
| Record name | Metformin [USAN:INN:BAN] | |
| Source | ChemIDplus | |
| URL | https://pubchem.ncbi.nlm.nih.gov/substance/?source=chemidplus&sourceid=0000657249 | |
| Description | ChemIDplus is a free, web search system that provides access to the structure and nomenclature authority files used for the identification of chemical substances cited in National Library of Medicine (NLM) databases, including the TOXNET system. | |
| Record name | Metformin | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00331 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Metformin | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID2023270 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
| Record name | Metformin | |
| Source | European Chemicals Agency (ECHA) | |
| URL | https://echa.europa.eu/substance-information/-/substanceinfo/100.010.472 | |
| Description | The European Chemicals Agency (ECHA) is an agency of the European Union which is the driving force among regulatory authorities in implementing the EU's groundbreaking chemicals legislation for the benefit of human health and the environment as well as for innovation and competitiveness. | |
| Explanation | Use of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page. | |
| Record name | METFORMIN | |
| Source | FDA Global Substance Registration System (GSRS) | |
| URL | https://gsrs.ncats.nih.gov/ginas/app/beta/substances/9100L32L2N | |
| Description | The FDA Global Substance Registration System (GSRS) enables the efficient and accurate exchange of information on what substances are in regulated products. Instead of relying on names, which vary across regulatory domains, countries, and regions, the GSRS knowledge base makes it possible for substances to be defined by standardized, scientific descriptions. | |
| Explanation | Unless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required. | |
| Record name | METFORMIN | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/7080 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
| Record name | 1,1-Dimethylbiguanide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0001921 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Melting Point |
223-226 °C, 223 - 226 °C | |
| Record name | Metformin | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00331 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | 1,1-Dimethylbiguanide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0001921 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Retrosynthesis Analysis
AI-Powered Synthesis Planning: Our tool employs the Template_relevance Pistachio, Template_relevance Bkms_metabolic, Template_relevance Pistachio_ringbreaker, Template_relevance Reaxys, Template_relevance Reaxys_biocatalysis model, leveraging a vast database of chemical reactions to predict feasible synthetic routes.
One-Step Synthesis Focus: Specifically designed for one-step synthesis, it provides concise and direct routes for your target compounds, streamlining the synthesis process.
Accurate Predictions: Utilizing the extensive PISTACHIO, BKMS_METABOLIC, PISTACHIO_RINGBREAKER, REAXYS, REAXYS_BIOCATALYSIS database, our tool offers high-accuracy predictions, reflecting the latest in chemical research and data.
Strategy Settings
| Precursor scoring | Relevance Heuristic |
|---|---|
| Min. plausibility | 0.01 |
| Model | Template_relevance |
| Template Set | Pistachio/Bkms_metabolic/Pistachio_ringbreaker/Reaxys/Reaxys_biocatalysis |
| Top-N result to add to graph | 6 |
Feasible Synthetic Routes
Disclaimer and Information on In-Vitro Research Products
Please be aware that all articles and product information presented on BenchChem are intended solely for informational purposes. The products available for purchase on BenchChem are specifically designed for in-vitro studies, which are conducted outside of living organisms. In-vitro studies, derived from the Latin term "in glass," involve experiments performed in controlled laboratory settings using cells or tissues. It is important to note that these products are not categorized as medicines or drugs, and they have not received approval from the FDA for the prevention, treatment, or cure of any medical condition, ailment, or disease. We must emphasize that any form of bodily introduction of these products into humans or animals is strictly prohibited by law. It is essential to adhere to these guidelines to ensure compliance with legal and ethical standards in research and experimentation.