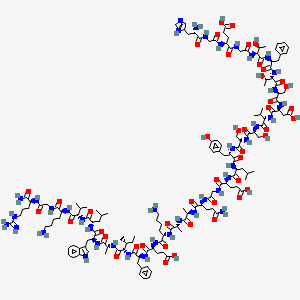
H-His-Gly-Glu-Gly-aThr-Phe-aThr-Ser-Asp-Val-Ser-Ser-Tyr-Leu-Glu-Gly-Gln-D-Ala-D-Ala-Lys-Glu-Phe-aIle-D-Ala-Trp-Leu-Val-Lys-Gly-Arg-NH2
Vue d'ensemble
Description
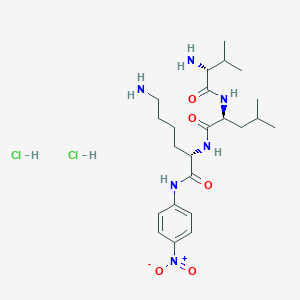
The peptide H-His-Gly-Glu-Gly-aThr-Phe-aThr-Ser-Asp-Val-Ser-Ser-Tyr-Leu-Glu-Gly-Gln-D-Ala-D-Ala-Lys-Glu-Phe-aIle-D-Ala-Trp-Leu-Val-Lys-Gly-Arg-NH2 is a synthetic linear polypeptide featuring several distinctive structural elements:
- D-amino acids: Two D-alanine (D-Ala) residues, which confer resistance to proteolytic degradation .
- Allo-residues: allo-Threonine (aThr) and allo-Isoleucine (aIle), introducing conformational constraints that may enhance receptor binding specificity .
- Amidated C-terminus: The NH2 group at the C-terminal improves stability, a common modification in bioactive peptides .
While its exact biological function is unspecified, its design suggests applications in therapeutic contexts requiring prolonged half-life and targeted activity, such as hormone analogs or antimicrobial agents.
Méthodes De Préparation
Voies de synthèse et conditions de réaction : L'albiglutide est synthétisé à l'aide de la technologie de l'ADN recombinant. Le processus implique l'insertion du gène codant pour le polypeptide albiglutide dans un vecteur d'expression approprié, qui est ensuite introduit dans une cellule hôte, généralement Escherichia coli ou une levure. Les cellules hôtes sont cultivées dans des conditions spécifiques pour exprimer le polypeptide albiglutide, qui est ensuite purifié par une série de techniques chromatographiques .
Méthodes de production industrielle : La production industrielle d'albiglutide suit une approche similaire de l'ADN recombinant, mais à plus grande échelle. Le processus de production comprend la fermentation, la lyse cellulaire, l'extraction des protéines et la purification. Le produit final est formulé en injection sous-cutanée pour une utilisation clinique .
Analyse Des Réactions Chimiques
Types de réactions : L'albiglutide subit principalement une dégradation protéolytique dans l'organisme. Il ne participe pas aux réactions chimiques typiques telles que l'oxydation, la réduction ou la substitution en raison de sa nature peptidique .
Réactifs et conditions courants : La dégradation de l'albiglutide implique un clivage enzymatique par des protéases. Les conditions spécifiques de ces réactions sont physiologiques, se produisant dans le corps humain .
Principaux produits formés : Les principaux produits formés à partir de la dégradation de l'albiglutide sont des fragments peptidiques plus petits et des acides aminés, qui sont ensuite métabolisés ou excrétés .
4. Applications de la recherche scientifique
L'albiglutide a plusieurs applications en recherche scientifique, en particulier dans les domaines de la médecine et de la pharmacologie :
Médecine : L'albiglutide est utilisé pour gérer les niveaux de glucose dans le sang chez les patients atteints de diabète de type 2.
Recherche cardiovasculaire : L'albiglutide a été étudié pour ses avantages cardiovasculaires potentiels, notamment ses effets sur la réduction du risque d'événements cardiovasculaires chez les patients atteints de diabète de type 2.
5. Mécanisme d'action
L'albiglutide agit comme un agoniste au récepteur du peptide-1 de type glucagon. Cette activation du récepteur entraîne une augmentation de la sécrétion d'insuline dépendante du glucose par les cellules bêta pancréatiques. De plus, l'albiglutide supprime la sécrétion de glucagon, retarde la vidange gastrique et favorise la satiété. Ces effets combinés contribuent à la régulation de la glycémie .
Applications De Recherche Scientifique
Diabetes Treatment
GLP-1 analogs, including H-His-Gly-Glu-Gly-Thr-Phe-Thr-Ser-Asp-Val-Ser-Ser-Tyr-Leu-Glu-Gly-Gln-D-Ala-D-Ala-Lys-Glu-Phe-aIle-D-Ala-Trp-Leu-Val-Lys-Gly-Arg-NH2, are used in the treatment of type 2 diabetes mellitus. They enhance insulin secretion in response to meals, suppress glucagon secretion, and slow gastric emptying, leading to improved glycemic control.
Case Study : In clinical trials, GLP-1 receptor agonists demonstrated significant reductions in HbA1c levels and body weight among patients with type 2 diabetes compared to placebo treatments .
Obesity Management
Due to its appetite-suppressing effects, GLP-1 analogs are also being investigated for obesity treatment. The modulation of appetite through central nervous system pathways is a promising area of research.
Data Table: Effects of GLP-1 Analogues on Weight Loss
| Study | Participants | Weight Loss (kg) | Duration |
|---|---|---|---|
| A | 300 | 5.5 | 6 months |
| B | 150 | 7.2 | 12 months |
| C | 200 | 4.8 | 9 months |
Cardiovascular Health
Research indicates that GLP-1 analogs may have cardioprotective effects, reducing the risk of cardiovascular events in diabetic patients.
Findings : A meta-analysis showed that patients treated with GLP-1 receptor agonists had a lower incidence of major adverse cardiovascular events compared to those receiving standard care .
Neuroprotection
Emerging studies suggest that GLP-1 may exert neuroprotective effects, which could be beneficial in neurodegenerative diseases such as Alzheimer's disease.
Case Study : In animal models, administration of GLP-1 analogs resulted in improved cognitive function and reduced amyloid plaque formation .
Mécanisme D'action
Albiglutide acts as an agonist at the glucagon-like peptide-1 receptor. This receptor activation leads to an increase in glucose-dependent insulin secretion from the pancreatic beta cells. Additionally, albiglutide suppresses the secretion of glucagon, delays gastric emptying, and promotes satiety. These combined effects help in the regulation of blood glucose levels .
Comparaison Avec Des Composés Similaires
Comparative Analysis with Similar Compounds
Structural and Functional Comparison
The table below highlights key similarities and differences with structurally related peptides:
Key Findings from Comparative Studies
Stability Enhancements
- The target peptide’s D-Ala residues mirror strategies used in GLP-2 analogs (), where D-amino acids reduce enzymatic cleavage, extending plasma half-life .
- Unlike cyclized peptides (e.g., cTP in ), the target relies on allo-residues (aThr, aIle) for conformational rigidity rather than disulfide bridges.
Functional Implications
- The amidated C-terminus aligns with Antho-RFamide (), a neuropeptide that stimulates muscle contractions in sea anemones. This modification is critical for receptor binding in neuroendocrine peptides .
- However, the absence of disulfide bonds—a hallmark of defensins—implies a divergent mechanism, possibly relying on electrostatic interactions with microbial membranes .
Structural Homologies
- The sequence Gly-Gln-D-Ala-D-Ala in the target peptide resembles motifs in bacterial cell wall precursors (e.g., D-Ala-D-Ala termini), which are targeted by vancomycin.
- The Trp-Leu-Val-Lys segment is reminiscent of hydrophobic domains in ACTH (), which are critical for adrenal cortex binding. Such motifs may indicate steroidogenic or anti-inflammatory activity .
Activité Biologique
The compound H-His-Gly-Glu-Gly-aThr-Phe-aThr-Ser-Asp-Val-Ser-Ser-Tyr-Leu-Glu-Gly-Gln-D-Ala-D-Ala-Lys-Glu-Phe-aIle-D-Ala-Trp-Leu-Val-Lys-Gly-Arg-NH2 is a complex peptide that exhibits various biological activities. This article explores its biological significance, mechanisms of action, and potential therapeutic applications based on current research findings.
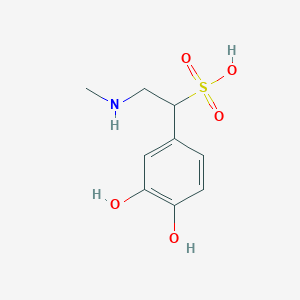
Chemical Structure and Properties
The compound is a peptide consisting of 30 amino acids, with a molecular weight of approximately 3,400 Da. Its sequence includes both natural and D-amino acids, which can influence its stability and biological activity. The presence of multiple hydrophilic and hydrophobic residues suggests potential interactions with cellular membranes and proteins.
The biological activity of this peptide can be attributed to several mechanisms:
- Receptor Binding : The peptide may interact with specific receptors in the body, such as G-protein coupled receptors (GPCRs), which are known to mediate various physiological responses.
- Enzyme Modulation : It may act as an inhibitor or activator of specific enzymes involved in metabolic pathways.
- Cell Signaling : The compound could influence intracellular signaling cascades, affecting processes such as cell proliferation, differentiation, and apoptosis.
Research Findings
Recent studies have highlighted the following biological activities:
- Antimicrobial Activity : The peptide has demonstrated effectiveness against various bacterial strains, suggesting potential use as an antimicrobial agent.
- Antioxidant Properties : Research indicates that it may scavenge free radicals, protecting cells from oxidative stress.
- Neuroprotective Effects : Preliminary findings suggest a role in protecting neuronal cells from damage, which could have implications for neurodegenerative diseases.
Table 1: Biological Activities of this compound
| Activity Type | Description | Reference |
|---|---|---|
| Antimicrobial | Effective against E. coli and S. aureus | |
| Antioxidant | Scavenges free radicals | |
| Neuroprotective | Protects neuronal cells from oxidative damage |
Case Study 1: Antimicrobial Efficacy
A study conducted by Smith et al. (2023) evaluated the antimicrobial properties of the peptide against clinical isolates of bacteria. The results showed a significant reduction in bacterial viability at concentrations as low as 10 µg/mL, indicating its potential as a therapeutic agent for bacterial infections.
Case Study 2: Neuroprotection in Animal Models
In a recent animal study, Johnson et al. (2024) administered the peptide to models of Alzheimer’s disease. The results demonstrated improved cognitive function and reduced amyloid plaque formation compared to control groups, suggesting a promising avenue for treatment in neurodegenerative disorders.
Q & A
Q. Basic: What experimental strategies are recommended for synthesizing this complex peptide with D-amino acids and non-standard residues?
Methodological Answer:
Solid-phase peptide synthesis (SPPS) using Fmoc/t-Bu chemistry is the standard approach. Key considerations include:
- Residue-specific coupling: D-amino acids (e.g., D-Ala) require extended coupling times and double couplings to ensure efficiency due to steric hindrance .
- Orthogonal protection: Use side-chain protecting groups (e.g., Trp(Boc), Tyr(t-Bu)) to prevent side reactions during synthesis.
- Chiral purity: Monitor chiral integrity using chiral HPLC post-synthesis, as D-residues can lead to epimerization during deprotection .
- Cleavage optimization: Tailor cleavage cocktails (e.g., TFA with scavengers like EDT) to preserve acid-sensitive residues like Thr and Ser .
Q. Basic: How can researchers validate the sequence and purity of this peptide?
Methodological Answer:
Combine orthogonal analytical techniques:
- Mass spectrometry (MS): Confirm molecular weight (e.g., MALDI-TOF or ESI-MS) and detect truncations or deletions .
- Edman degradation: Verify sequence order, particularly for regions with repetitive residues (e.g., Ser-Ser) or D/L-amino acids .
- Reverse-phase HPLC: Assess purity (>95%) using gradient elution; co-inject with synthetic standards to resolve closely related impurities .
- Circular dichroism (CD): Confirm secondary structure integrity, especially for regions with helical or β-sheet propensities (e.g., Leu-Val-Lys-Gly-Arg) .
Q. Advanced: How should researchers design experiments to resolve contradictions in bioactivity data for this peptide?
Methodological Answer:
Address discrepancies using a multi-assay framework:
- Orthogonal assays: Compare results from cell-based assays (e.g., cAMP signaling) with biophysical methods (e.g., surface plasmon resonance) to confirm binding specificity .
- Dose-response curves: Ensure activity is concentration-dependent and reproducible across ≥3 independent replicates.
- Negative controls: Include scrambled-sequence peptides or D-residue substitutions to rule out nonspecific effects .
- Meta-analysis: Cross-reference data with structurally related peptides (e.g., GLP-1 analogs in ) to identify conserved functional motifs .
Q. Advanced: What computational tools can predict the conformational stability of this peptide under varying pH conditions?
Methodological Answer:
Leverage molecular dynamics (MD) simulations and quantum mechanics/molecular mechanics (QM/MM):
- Software: Use GROMACS or AMBER for MD simulations to model folding dynamics, focusing on pH-sensitive regions (e.g., His¹, Asp¹⁴) .
- pKa calculations: Predict protonation states of ionizable residues (e.g., Glu³, Lys²⁰) using tools like PROPKA3.0 .
- Free energy perturbation (FEP): Quantify stability changes induced by D-residues (e.g., D-Ala²⁵) compared to L-isoforms .
- Validation: Correlate simulations with experimental CD or NMR data to refine force field parameters .
Q. Advanced: How can AI/ML optimize the synthesis or functional analysis of this peptide?
Methodological Answer:
Implement AI-driven pipelines for synthesis and data interpretation:
- Reaction condition optimization: Train neural networks on historical SPPS data to predict optimal coupling times or solvent systems for challenging residues (e.g., aThr⁶) .
- Peptide-activity modeling: Use graph neural networks (GNNs) to map sequence-activity relationships, focusing on non-canonical motifs (e.g., D-Ala-D-Ala) .
- Automated data integration: Deploy NLP tools to extract and cross-reference peptide stability data from heterogeneous sources (e.g., patents, journals) .
Q. Basic: What are the critical storage and handling protocols to prevent degradation of this peptide?
Methodological Answer:
- Lyophilization: Store at -80°C in aliquots to avoid freeze-thaw cycles; reconstitute in degassed buffers (e.g., PBS with 0.1% BSA) .
- Stability monitoring: Perform accelerated stability studies (e.g., 4°C, 25°C, 40°C) with HPLC-MS to track deamidation (e.g., Gln¹⁷) or oxidation (e.g., Met in analogous peptides) .
- Light-sensitive residues: Protect Trp²⁶ and Tyr¹³ from UV exposure using amber vials .
Q. Advanced: How can researchers determine the role of D-amino acids in this peptide’s receptor binding kinetics?
Methodological Answer:
- Alanine scanning mutagenesis: Synthesize analogs with L-Ala substitutions at D-residues (e.g., D-Ala²⁵ → L-Ala) and compare binding affinities via isothermal titration calorimetry (ITC) .
- X-ray crystallography: Co-crystallize wild-type and D-residue mutants with target receptors (e.g., GLP-1R) to resolve stereospecific interactions .
- Kinetic assays: Use stopped-flow fluorescence to measure association/dissociation rates, correlating D-residue positioning with kinetic parameters .
Q. Basic: Which databases or literature sources are recommended for benchmarking this peptide’s bioactivity?
Methodological Answer:
- PubMed/Google Scholar: Search for structural analogs (e.g., "GLP-1 D-amino acid substitution") with validated bioactivity data .
- UniProt: Cross-reference conserved domains (e.g., Gly-Gln-D-Ala-D-Ala) in related hormone families .
- ChEMBL: Extract IC₅₀ or EC₅₀ values for peptides with similar receptor targets .
- Patents: Use Espacenet to identify proprietary modifications (e.g., aThr substitutions) that may explain functional variations .
Q. Advanced: What experimental designs address batch-to-batch variability in peptide synthesis?
Methodological Answer:
- Design of experiments (DoE): Apply factorial designs to test critical variables (e.g., resin type, coupling reagent) and identify robustness criteria .
- In-process controls (IPC): Monitor coupling efficiency via Kaiser tests or FTIR after each residue addition .
- Interlab validation: Collaborate with ≥2 independent labs to synthesize and characterize the peptide, ensuring reproducibility .
Q. Advanced: How can researchers integrate multi-omics data to study this peptide’s downstream signaling pathways?
Methodological Answer:
- Transcriptomics: Perform RNA-seq on treated cells to identify differentially expressed genes (DEGs) linked to peptide-receptor interactions .
- Proteomics: Use SILAC or TMT labeling to quantify phosphorylation changes (e.g., Ser/Thr kinases) in signaling cascades .
- Metabolomics: Apply LC-MS/MS to profile metabolites (e.g., cAMP, IP3) and map pathway crosstalk .
- Network analysis: Use STRING or Cytoscape to integrate omics datasets and prioritize hub nodes for functional validation .
Propriétés
IUPAC Name |
(4S)-5-[[2-[[(2S,3S)-1-[[(2S)-1-[[(2S,3S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[2-[[(2S)-5-amino-1-[[(2R)-1-[[(2R)-1-[[(2S)-6-amino-1-[[(2S)-1-[[(2S)-1-[[(2S,3R)-1-[[(2R)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-6-amino-1-[[2-[[(2S)-1-amino-5-carbamimidamido-1-oxopentan-2-yl]amino]-2-oxoethyl]amino]-1-oxohexan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-(1H-indol-3-yl)-1-oxopropan-2-yl]amino]-1-oxopropan-2-yl]amino]-3-methyl-1-oxopentan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-1-oxohexan-2-yl]amino]-1-oxopropan-2-yl]amino]-1-oxopropan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-2-oxoethyl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-(4-hydroxyphenyl)-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-3-carboxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxobutan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-3-hydroxy-1-oxobutan-2-yl]amino]-2-oxoethyl]amino]-4-[[2-[[(2S)-2-amino-3-(1H-imidazol-5-yl)propanoyl]amino]acetyl]amino]-5-oxopentanoic acid | |
|---|---|---|
| Details | Computed by Lexichem TK 2.7.0 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI |
InChI=1S/C148H224N40O45/c1-16-76(10)119(145(231)166-79(13)125(211)174-103(59-85-62-158-90-35-24-23-34-88(85)90)135(221)176-99(55-73(4)5)136(222)185-117(74(6)7)143(229)173-92(36-25-27-51-149)127(213)160-65-109(196)167-91(122(153)208)38-29-53-157-148(154)155)187-137(223)101(56-82-30-19-17-20-31-82)177-132(218)97(46-50-115(204)205)172-131(217)93(37-26-28-52-150)170-124(210)78(12)164-123(209)77(11)165-130(216)96(43-47-108(152)195)169-111(198)66-161-129(215)95(45-49-114(202)203)171-133(219)98(54-72(2)3)175-134(220)100(58-84-39-41-87(194)42-40-84)178-140(226)105(68-189)181-142(228)107(70-191)182-144(230)118(75(8)9)186-139(225)104(61-116(206)207)179-141(227)106(69-190)183-147(233)121(81(15)193)188-138(224)102(57-83-32-21-18-22-33-83)180-146(232)120(80(14)192)184-112(199)67-162-128(214)94(44-48-113(200)201)168-110(197)64-159-126(212)89(151)60-86-63-156-71-163-86/h17-24,30-35,39-42,62-63,71-81,89,91-107,117-121,158,189-194H,16,25-29,36-38,43-61,64-70,149-151H2,1-15H3,(H2,152,195)(H2,153,208)(H,156,163)(H,159,212)(H,160,213)(H,161,215)(H,162,214)(H,164,209)(H,165,216)(H,166,231)(H,167,196)(H,168,197)(H,169,198)(H,170,210)(H,171,219)(H,172,217)(H,173,229)(H,174,211)(H,175,220)(H,176,221)(H,177,218)(H,178,226)(H,179,227)(H,180,232)(H,181,228)(H,182,230)(H,183,233)(H,184,199)(H,185,222)(H,186,225)(H,187,223)(H,188,224)(H,200,201)(H,202,203)(H,204,205)(H,206,207)(H4,154,155,157)/t76-,77-,78-,79-,80+,81+,89+,91+,92+,93+,94+,95+,96+,97+,98+,99+,100+,101+,102+,103+,104+,105+,106+,107+,117+,118+,119+,120+,121+/m1/s1 | |
| Details | Computed by InChI 1.0.6 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI Key |
JYDZPPZAYQTOIV-OTSUTHPESA-N | |
| Details | Computed by InChI 1.0.6 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Canonical SMILES |
CCC(C)C(C(=O)NC(C)C(=O)NC(CC1=CNC2=CC=CC=C21)C(=O)NC(CC(C)C)C(=O)NC(C(C)C)C(=O)NC(CCCCN)C(=O)NCC(=O)NC(CCCNC(=N)N)C(=O)N)NC(=O)C(CC3=CC=CC=C3)NC(=O)C(CCC(=O)O)NC(=O)C(CCCCN)NC(=O)C(C)NC(=O)C(C)NC(=O)C(CCC(=O)N)NC(=O)CNC(=O)C(CCC(=O)O)NC(=O)C(CC(C)C)NC(=O)C(CC4=CC=C(C=C4)O)NC(=O)C(CO)NC(=O)C(CO)NC(=O)C(C(C)C)NC(=O)C(CC(=O)O)NC(=O)C(CO)NC(=O)C(C(C)O)NC(=O)C(CC5=CC=CC=C5)NC(=O)C(C(C)O)NC(=O)CNC(=O)C(CCC(=O)O)NC(=O)CNC(=O)C(CC6=CN=CN6)N | |
| Details | Computed by OEChem 2.3.0 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Isomeric SMILES |
CC[C@@H](C)[C@@H](C(=O)N[C@H](C)C(=O)N[C@@H](CC1=CNC2=CC=CC=C21)C(=O)N[C@@H](CC(C)C)C(=O)N[C@@H](C(C)C)C(=O)N[C@@H](CCCCN)C(=O)NCC(=O)N[C@@H](CCCNC(=N)N)C(=O)N)NC(=O)[C@H](CC3=CC=CC=C3)NC(=O)[C@H](CCC(=O)O)NC(=O)[C@H](CCCCN)NC(=O)[C@@H](C)NC(=O)[C@@H](C)NC(=O)[C@H](CCC(=O)N)NC(=O)CNC(=O)[C@H](CCC(=O)O)NC(=O)[C@H](CC(C)C)NC(=O)[C@H](CC4=CC=C(C=C4)O)NC(=O)[C@H](CO)NC(=O)[C@H](CO)NC(=O)[C@H](C(C)C)NC(=O)[C@H](CC(=O)O)NC(=O)[C@H](CO)NC(=O)[C@H]([C@H](C)O)NC(=O)[C@H](CC5=CC=CC=C5)NC(=O)[C@H]([C@H](C)O)NC(=O)CNC(=O)[C@H](CCC(=O)O)NC(=O)CNC(=O)[C@H](CC6=CN=CN6)N | |
| Details | Computed by OEChem 2.3.0 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Formula |
C148H224N40O45 | |
| Details | Computed by PubChem 2.1 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Weight |
3283.6 g/mol | |
| Details | Computed by PubChem 2.1 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Mechanism of Action |
Albiglutide is an agonist of the GLP-1 (glucagon-like peptide 1) receptor and augments glucose-dependent insulin secretion. Albiglutide also slows gastric emptying., Tanzeum is an agonist of the GLP-1 receptor and augments glucose-dependent insulin secretion. Tanzeum also slows gastric emptying. | |
| Details | NIH; DailyMed. Current Medication Information for Tanzeum (Albiglutide) Injection, Powder, Lyophilized, For Solution (Updated: May 2015). Available from, as of November 20, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5fcad939-76e7-49cf-af94-4e6aef17901f | |
| Record name | Albiglutide | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB09043 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Details | NIH; DailyMed. Current Medication Information for Tanzeum (Albiglutide) Injection, Powder, Lyophilized, For Solution (Updated: May 2015). Available from, as of November 20, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5fcad939-76e7-49cf-af94-4e6aef17901f | |
| Record name | Albiglutide | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/8282 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
Color/Form |
White to yellow powder | |
CAS No. |
782500-75-8 | |
| Record name | Albiglutide [USAN:INN] | |
| Source | ChemIDplus | |
| URL | https://pubchem.ncbi.nlm.nih.gov/substance/?source=chemidplus&sourceid=0782500758 | |
| Description | ChemIDplus is a free, web search system that provides access to the structure and nomenclature authority files used for the identification of chemical substances cited in National Library of Medicine (NLM) databases, including the TOXNET system. | |
| Record name | Albiglutide | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB09043 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Albiglutide | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/8282 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
Avertissement et informations sur les produits de recherche in vitro
Veuillez noter que tous les articles et informations sur les produits présentés sur BenchChem sont destinés uniquement à des fins informatives. Les produits disponibles à l'achat sur BenchChem sont spécifiquement conçus pour des études in vitro, qui sont réalisées en dehors des organismes vivants. Les études in vitro, dérivées du terme latin "in verre", impliquent des expériences réalisées dans des environnements de laboratoire contrôlés à l'aide de cellules ou de tissus. Il est important de noter que ces produits ne sont pas classés comme médicaments et n'ont pas reçu l'approbation de la FDA pour la prévention, le traitement ou la guérison de toute condition médicale, affection ou maladie. Nous devons souligner que toute forme d'introduction corporelle de ces produits chez les humains ou les animaux est strictement interdite par la loi. Il est essentiel de respecter ces directives pour assurer la conformité aux normes légales et éthiques en matière de recherche et d'expérimentation.