Tramadol
Overview
Description
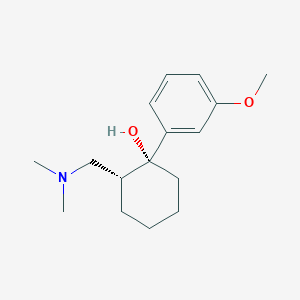
Tramadol is a centrally acting analgesic used to treat moderate to severe pain. It is an opioid pain medication and a serotonin-norepinephrine reuptake inhibitor. This compound is available in various forms, including tablets, capsules, and injections. It was first introduced in 1977 by the German pharmaceutical company Grünenthal GmbH under the brand name "Tramal" .
Preparation Methods
Synthetic Routes and Reaction Conditions
The synthesis of tramadol involves several steps. One common method starts with the reaction of 3-methoxyphenylmagnesium bromide with cyclohexanone to form 1-(3-methoxyphenyl)cyclohexanol. This intermediate is then reacted with dimethylamine to produce this compound .
Industrial Production Methods
In industrial settings, this compound hydrochloride is often prepared using a one-pot process. This involves reacting a mixture of (RR,SS)- and (RS,SR)-2-dimethylaminomethyl-1-(3-methoxyphenyl)cyclohexanol with hydrochloric acid in the presence of a catalytic amount of water. This method is advantageous as it avoids the use of carcinogenic solvents and simplifies the production process .
Chemical Reactions Analysis
Types of Reactions
Tramadol undergoes several types of chemical reactions, including:
Reduction: Reduction reactions are less common but can occur under specific conditions.
Substitution: this compound can undergo substitution reactions, particularly in the presence of strong nucleophiles.
Common Reagents and Conditions
Oxidation: Common oxidizing agents include potassium permanganate and hydrogen peroxide.
Reduction: Reducing agents such as lithium aluminum hydride can be used.
Substitution: Strong nucleophiles like sodium hydride can facilitate substitution reactions.
Major Products
The major products formed from these reactions include O-desmethylthis compound and various substituted derivatives, depending on the reagents and conditions used .
Scientific Research Applications
Pharmacological Profile
Tramadol acts as a mu-opioid receptor agonist and a serotonin-norepinephrine reuptake inhibitor (SNRI) , which contributes to its analgesic effects. It is primarily used for the treatment of moderate to severe pain, including:
- Postoperative pain
- Chronic pain syndromes (e.g., rheumatoid arthritis, fibromyalgia)
- Neuropathic pain
- Labor pain
- Osteoarthritis and cancer-related pain
This compound's analgesic potency is approximately one-tenth that of morphine, making it a valuable option for patients who require effective pain control without the higher risks associated with stronger opioids .
Pain Management
This compound is indicated for:
- Acute Pain: Effective in managing postoperative and injury-related pain.
- Chronic Pain: Often prescribed for conditions like fibromyalgia and chronic back pain, where it serves as a second-line treatment option .
The drug's unique mechanism allows it to address both nociceptive and neuropathic pain pathways, making it suitable for diverse patient populations .
Off-Label Uses
This compound has also been explored for various off-label applications:
- Restless Legs Syndrome (RLS): It is occasionally prescribed for refractory cases where first-line treatments fail .
- Premature Ejaculation: Some studies suggest this compound's efficacy in delaying ejaculation, although this use remains controversial .
- Psychiatric Disorders: There is emerging interest in this compound's potential antidepressant effects, warranting further investigation into its use in psychiatric care .
Pharmacokinetics and Dosing
This compound is rapidly absorbed after oral administration, with peak plasma concentrations occurring within 1.6 to 2 hours. The recommended dosing regimen typically involves:
| Formulation | Dosage Range | Frequency |
|---|---|---|
| Immediate Release | 50–100 mg every 4–6 hours | As needed |
| Extended Release | 200 mg once daily | Daily |
The bioavailability of this compound is approximately 75%, influenced by first-pass metabolism .
Efficacy in Pain Management
A systematic review highlighted this compound's effectiveness across various pain types, noting its role in postoperative settings and chronic pain management. A study indicated that patients with fibromyalgia experienced significant relief when this compound was included in their treatment regimen .
Abuse Potential
Despite its therapeutic benefits, this compound has been associated with abuse potential. Research indicates that while it poses a lower risk of addiction compared to traditional opioids, misuse has been documented, particularly among young adults. This necessitates careful monitoring when prescribing this compound .
Mechanism of Action
Tramadol exerts its effects through multiple mechanisms:
Opioid Receptor Activation: This compound binds to the μ-opioid receptor, although with lower affinity compared to other opioids.
Monoamine Reuptake Inhibition: This compound inhibits the reuptake of serotonin and norepinephrine, enhancing their levels in the synaptic cleft and contributing to its analgesic effects.
Ion Channel Modulation: This compound affects ion channels, particularly voltage-gated sodium channels, which play a role in pain signaling.
Comparison with Similar Compounds
Similar Compounds
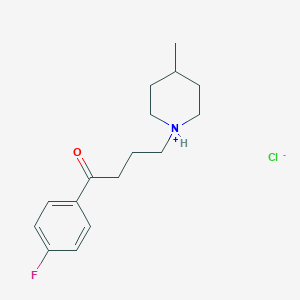
Codeine: Like tramadol, codeine is an opioid used for pain relief.
Morphine: Morphine is a stronger opioid compared to this compound and is used for severe pain.
Tapentadol: Tapentadol is similar to this compound but is stronger and has a different regulatory classification.
Uniqueness
This compound’s uniqueness lies in its dual mechanism of action, combining opioid receptor activation with monoamine reuptake inhibition. This makes it effective for a wide range of pain types and provides additional benefits such as anxiolytic and antidepressant effects .
Biological Activity
Tramadol is a synthetic opioid analgesic widely used for managing moderate to severe pain. Its biological activity is characterized by a complex mechanism involving multiple pathways, including opioid receptor agonism, serotonin and norepinephrine reuptake inhibition, and modulation of various pain pathways. This article provides a detailed overview of this compound's biological activity, including its pharmacokinetics, pharmacodynamics, and associated clinical findings.
This compound operates primarily through:
- Opioid Receptor Agonism : this compound binds to the μ-opioid receptors (μ-OR), which are crucial for its analgesic effects. The primary active metabolite, O-desmethylthis compound (M1), exhibits significantly higher potency at these receptors—up to 200 times more than this compound itself .
- Serotonin and Norepinephrine Reuptake Inhibition : this compound also functions as a serotonin-norepinephrine reuptake inhibitor (SNRI), enhancing the levels of these neurotransmitters in the synaptic cleft, which contributes to its analgesic properties .
- Interaction with Other Receptors : It influences various other receptor systems, including alpha2-adrenoreceptors and NMDA receptors, which play roles in modulating pain perception .
Pharmacokinetics
This compound is rapidly absorbed after oral administration, with peak plasma concentrations typically reached within 1.6 to 3 hours. The bioavailability is approximately 75%, influenced by first-pass metabolism in the liver . The following table summarizes key pharmacokinetic parameters:
| Parameter | Value |
|---|---|
| Bioavailability | ~75% |
| Peak Plasma Concentration (Cmax) | ~300 μg/L |
| Time to Peak Concentration (Tmax) | 1.6 - 3 hours |
| Elimination Half-life | 5-6 hours |
Genetic Factors Influencing Response
The variability in this compound response can be attributed to genetic polymorphisms in the cytochrome P450 enzyme system, particularly CYP2D6. Individuals with different CYP2D6 genotypes exhibit significant differences in this compound metabolism and efficacy:
- Extensive Metabolizers (EM) : Normal function of CYP2D6 leads to effective conversion to M1.
- Poor Metabolizers (PM) : Reduced or absent CYP2D6 function results in lower M1 levels and potentially less effective pain relief .
Efficacy and Safety
A study involving over 88,000 patients indicated that this compound use was associated with higher all-cause mortality rates compared to naproxen and diclofenac. The hazard ratio for this compound was found to be significantly elevated (HR = 1.71 compared to naproxen) during a one-year follow-up period .
Chronic Use Effects
Research on chronic this compound use has demonstrated adverse histopathological changes in animal models. A study on rats showed significant oxidative stress markers and increased apoptosis in brain and testicular tissues after prolonged this compound administration . The findings suggest potential long-term effects on fertility and psychological health.
Summary of Research Findings
Recent studies have highlighted the multifaceted biological activity of this compound, revealing both therapeutic benefits and risks associated with its use. Key findings include:
- Increased Risk of Dementia : A retrospective cohort study found a dose-response relationship between this compound use and the incidence of all-cause dementia among older adults .
- Neurotransmitter Disruption : Chronic exposure has been linked to alterations in neurotransmitter systems, evidenced by metabolomic analyses showing significant biomarker changes related to brain function .
Q & A
Basic Research Questions
Q. What are the primary pharmacological mechanisms of tramadol, and how do they influence experimental design in pain management studies?
this compound exerts dual mechanisms: weak µ-opioid receptor agonism and inhibition of serotonin/noradrenaline reuptake. Researchers must account for both pathways when designing studies, particularly when comparing this compound to pure opioids (e.g., morphine) or non-opioid analgesics. For example, preclinical studies should include assays for opioid receptor binding and neurotransmitter uptake inhibition . Clinical trials should stratify participants based on CYP2D6 polymorphisms, as this compound's active metabolite (O-desmethylthis compound) depends on this enzyme .
Q. How do researchers quantify this compound and its metabolites in biological samples?
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is the gold standard for detecting this compound and its 24+ metabolites in urine or plasma. Key parameters include:
- Chromatographic separation using reversed-phase columns (e.g., C18) with gradient elution .
- Internal standards (e.g., deuterated this compound) to correct for matrix effects .
- Validation per FDA guidelines, with limits of detection (LOD) ≤2.5 µg/L in urine .
Q. What are standard protocols for assessing this compound’s efficacy in cancer pain management?
The Cochrane Collaboration recommends:
- Study design : Randomized controlled trials (RCTs) with active comparators (e.g., morphine, codeine) and placebo controls.
- Outcomes : Pain reduction ≥30% from baseline, patient-reported "much improved" status, and adverse event rates (e.g., nausea, dizziness).
- Dosing : 50–600 mg/day, with titration based on pain severity .
Advanced Research Questions
Q. How can researchers resolve heterogeneity in meta-analyses of this compound for premature ejaculation (PE)?
Heterogeneity arises from variable dosing (25–100 mg on-demand), trial durations (1 day–6 months), and outcome measures (e.g., intravaginal ejaculatory latency time). Mitigation strategies include:
- Subgroup analysis by dose and administration frequency .
- Sensitivity analysis excluding open-label studies .
- Standardized reporting using CONSORT guidelines to reduce bias .
Q. What methodologies address conflicting data on this compound’s association with all-cause mortality in osteoarthritis patients?
A 2019 propensity score-matched cohort study found this compound increased mortality risk vs. NSAIDs (HR: 1.71–2.04) but not vs. codeine. To reconcile contradictions:
- Use instrumental variable analysis to adjust for unmeasured confounders (e.g., baseline pain severity).
- Conduct dose-response studies to differentiate risks between low-dose (50 mg/day) and high-dose regimens (≥300 mg/day) .
Q. How can mixed-methods approaches elucidate this compound abuse drivers in specific populations?
Combining qualitative discourse analysis (e.g., coding media narratives on this compound use in Ghana) with quantitative surveys identifies cultural and socioeconomic factors. For example:
- NVivo software for thematic analysis of 295 newspaper articles .
- Validated questionnaires assessing poly-substance use patterns (e.g., this compound + energy drinks) .
Q. What experimental models validate this compound’s off-label antidepressant effects?
Preclinical models:
- Forced swim test (FST) in rodents to assess serotonin/noradrenaline-mediated antidepressant activity.
- Microdialysis to measure extracellular monoamine levels in the prefrontal cortex . Clinical data mining:
- Analysis of patient-reported outcomes (e.g., 94.6% efficacy in 130 users) via platforms like Drugs.com .
Q. Methodological Challenges
Q. How to optimize LC-MS/MS for this compound metabolite profiling in complex matrices?
- Surfactant-assisted microextraction : Triton X-100 enhances recovery from blood or urine by 391–466× .
- Multivariate optimization : Design-of-experiment (DoE) approaches to balance pH, temperature, and salt content .
Q. What are ethical considerations in studying this compound’s performance-enhancing effects in athletes?
- Blinding protocols : Use placebo-controlled trials to avoid bias in cycling time-trial studies .
- Regulatory alignment : Align with UCI/WADA guidelines, even for non-prohibited substances (e.g., this compound’s 2019 monitoring phase) .
Q. Contradictory Findings and Solutions
Q. Why do animal models show divergent this compound pharmacokinetics vs. humans?
- Species differences : Dogs exhibit faster this compound clearance (54.63 mL/kg/min) vs. humans (6–8 mL/kg/min) due to CYP2D6 variability. Use transgenic rodent models expressing human CYP2D6 for translatability .
Q. How to interpret this compound’s abuse potential given conflicting DEA and epidemiological data?
- DEA classification : Schedule IV (low abuse risk) based on propoxyphene comparability .
- Field data : African studies report 20–60% nonmedical use rates, driven by lax regulation. Hybrid studies combining urine toxicology (LC-MS/MS) and geospatial analysis are critical .
Q. Tables for Key Data
Properties
IUPAC Name |
(1R,2R)-2-[(dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexan-1-ol | |
|---|---|---|
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI |
InChI=1S/C16H25NO2/c1-17(2)12-14-7-4-5-10-16(14,18)13-8-6-9-15(11-13)19-3/h6,8-9,11,14,18H,4-5,7,10,12H2,1-3H3/t14-,16+/m1/s1 | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI Key |
TVYLLZQTGLZFBW-ZBFHGGJFSA-N | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Canonical SMILES |
CN(C)CC1CCCCC1(C2=CC(=CC=C2)OC)O | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Isomeric SMILES |
CN(C)C[C@H]1CCCC[C@@]1(C2=CC(=CC=C2)OC)O | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Formula |
C16H25NO2 | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
DSSTOX Substance ID |
DTXSID90858931, DTXSID401167150 | |
| Record name | Tramadol | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID90858931 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
| Record name | (1R,2R)-2-[(Dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexanol | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID401167150 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
Molecular Weight |
263.37 g/mol | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Physical Description |
Solid | |
| Record name | Tramadol | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0014339 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Solubility |
>39.5 [ug/mL] (The mean of the results at pH 7.4), Soluble, 7.50e-01 g/L | |
| Record name | SID26663897 | |
| Source | Burnham Center for Chemical Genomics | |
| URL | https://pubchem.ncbi.nlm.nih.gov/bioassay/1996#section=Data-Table | |
| Description | Aqueous solubility in buffer at pH 7.4 | |
| Record name | Tramadol | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00193 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Tramadol | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0014339 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Mechanism of Action |
Tramadol is a centrally acting μ-opioid receptor agonist and SNRI (serotonin/norepinephrine reuptake-inhibitor) that is structurally related to [codeine] and [morphine]. Tramadol binds weakly to κ- and δ-opioid receptors and to the μ-opioid receptor with 6000-fold less affinity than morphine. Tramadol exists as a racemic mixture consisting of two pharmacologically active enantiomers that both contribute to its analgesic property through different mechanisms: (+)-tramadol and its primary metabolite (+)-O-desmethyl-tramadol (M1) are agonists of the μ opioid receptor while (+)-tramadol inhibits serotonin reuptake and (-)-tramadol inhibits norepinephrine reuptake. These pathways are complementary and synergistic, improving tramadol's ability to modulate the perception of and response to pain. In animal models, M1 is up to 6 times more potent than tramadol in producing analgesia and 200 times more potent in μ-opioid binding. Tramadol has also been shown to affect a number of pain modulators including alpha2-adrenoreceptors, neurokinin 1 receptors, the voltage-gated sodium channel type II alpha subunit, transient receptor potential cation channel subfamily V member 1 (TRPV1 - also known as the capsaicin receptor), muscarinic receptors (M1 and M3), N-methyl-D-aspartate receptor (also known as the NMDA receptor or glutamate receptor), Adenosine A1 receptors, and nicotinic acetylcholine receptor. In addition to the above neuronal targets, tramadol has a number of effects on inflammatory and immune mediators involved in the pain response. This includes inhibitory effects on cytokines, prostaglandin E2 (PGE2), nuclear factor-κB, and glial cells as well as a change in the polarization state of M1 macrophages., Tramadol is a racemic mixture (R & S) that has a complicated mechanism of action. It has some mu-opioid receptor action, but this effect is 10 times lower than codeine and 6000 timex lower than morphine. Tramadol also inhibits the reuptake of norepinephrine (NE) and serotonin (5 HT) and produces secondary effects on alpha-2 adrenergic receptors in pain pathways. One isomer has greater effect on 5 HT reuptake and greater affinity for mu-opiate receptors. The other isomer is more potent for NE reuptake and less active for inhibiting 5 HT reuptake. Taken together, the effects of of tramadol may be explained through inhibition of 5 HT reuptake, action on alpha2 receptors, and mild activity on opiate mu-receptors., The transient receptor potential vanilloid 1 (TRPV1) and the transient receptor potential ankyrin 1 (TRPA1), which are expressed in sensory neurons, are polymodal nonselective cation channels that sense noxious stimuli. Recent reports showed that these channels play important roles in inflammatory, neuropathic, or cancer pain, suggesting that they may serve as attractive analgesic pharmacological targets. Tramadol is an effective analgesic that is widely used in clinical practice. Reportedly, tramadol and its metabolite (M1) bind to mu-opioid receptors and/or inhibit reuptake of monoamines in the central nervous system, resulting in the activation of the descending inhibitory system. However, the fundamental mechanisms of tramadol in pain control remain unclear. TRPV1 and TRPA1 may be targets of tramadol; however, they have not been studied extensively. We examined whether and how tramadol and M1 act on human embryonic kidney 293 (HEK293) cells expressing human TRPV1 (hTRPV1) or hTRPA1 by using a Ca imaging assay and whole-cell patch-clamp recording. Tramadol and M1 (0.01-10 uM) alone did not increase in intracellular Ca concentration ([Ca]i) in HEK293 cells expressing hTRPV1 or hTRPA1 compared with capsaicin (a TRPV1 agonist) or the allyl isothiocyanate (AITC, a TRPA1 agonist), respectively. Furthermore, in HEK293 cells expressing hTRPV1, pretreatment with tramadol or M1 for 5 minutes did not change the increase in [Ca]i induced by capsaicin. Conversely, pretreatment with tramadol (0.1-10 uM) and M1 (1-10 uM) significantly suppressed the AITC-induced [Ca]i increases in HEK293 cells expressing hTRPA1. In addition, the patch-clamp study showed that pretreatment with tramadol and M1 (10 uM) decreased the inward currents induced by AITC. These data indicate that tramadol and M1 selectively inhibit the function of hTRPA1, but not that of hTRPV1, and that hTRPA1 may play a role in the analgesic effects of these compounds., Tramadol is an effective analgesic substance widely used in medical practice. Its therapeutic action have been mainly attributed to the activation of mu-opioid receptors as well as to the inhibition of neurotransmitter reuptake mechanisms and various voltage- and ligand-gated ion channels of the nociceptive system. As transient receptor potential vanilloid-1 (TRPV1, "the capsaicin receptor") has been shown to function as a central integrator molecule of pain sensation, our aim in the current study was to define the involvement of TRPV1 in the complex mechanism of action of tramadol. To achieve these goals, we used single-cell Ca-imaging as well as fluorescent image plate reader assays on Chinese hamster ovary (CHO) cells heterologously over-expressing TRPV1. We found that (1) tramadol, similar to the well-known TRPV1 agonist, capsaicin, significantly increased [Ca(2+)](i) of TRPV1-CHO cells in a concentration-dependent fashion; (2) its effect was reversibly prevented by the TRPV1 antagonist capsazepine; (3) repeated application of tramadol resulted in marked tachyphylaxis; and (4) tramadol did not modify [Ca(2+)](i) in control (empty vector expressing) CHO cells. Collectively, these findings strongly support the intriguing and novel concept that tramadol acts as an agonist of TRPV1. Considering that activation of TRPV1 on sensory neurons is followed by a local release of vasoactive neuropeptides and a marked desensitization of the afferent fibers (hence termination of pain sensation), our findings may equally explain both the desired analgesic as well as the often-seen, yet "unexpected," local side effects (e.g., initiation of burning pain and erythema) of tramadol., Tramadol has a dual mechanism of action that includes weak agonistic effects at the mu-opioid receptor as well as inhibition of monoamine (serotonin, norepinephrine) re-uptake. Its major (M1) metabolite mono-O:-desmethyltramadol, which is rapidly formed in vivo, has a markedly higher affinity for mu receptors and may thus contribute to the effects of the parent compound. Furthermore, the pharmacological effects of tramadol appear to be related to the different, but complementary and interactive pharmacologies of its enantiomers., Tramadol has been used as an analgesic for several decades. mu-Opioid receptors (muORs) are the major receptors that mediate the analgesic effects of opioids. Although muORs have been thought to be one of the sites of action of tramadol, there has been no report that directly proves whether tramadol is an agonist of muOR or not. In this study, we examined the effects of tramadol and its main active metabolite O-desmethyltramadol (M1), on the function of muORs using Xenopus oocytes expressing cloned human muORs. The effects of tramadol and M1 were evaluated using the Ca(2+)-activated Cl(-) current assay method for G(i/o)-protein-coupled receptors by using a muOR fused to G(qi5) (muOR-G(qi5)) in Xenopus oocytes. DAMGO [(D-Ala(2), N-MePhe(4), Gly(5)-ol)-enkephalin] evoked Cl(-) currents in oocytes expressing muOR-G(qi5) in a concentration-dependent manner. Tramadol and M1 also evoked Cl(-) currents in the oocytes expressing muOR-G(qi5); however, relatively higher concentrations (compared to DMAGO) were necessary to induce such currents. Tramadol and M1 had a direct effect on muORs expressed in Xenopus oocytes. Although the monoamine uptake system and several types of ligand-gated ion channels are thought to be one of the targets for tramadol, tramadol-induced antinociception may be mediated at least in part, by the direct activation of muORs. | |
| Record name | Tramadol | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00193 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | TRAMADOL | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/7047 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
CAS No. |
123154-38-1, 27203-92-5 | |
| Record name | (1R,2R)-2-[(Dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexanol | |
| Source | CAS Common Chemistry | |
| URL | https://commonchemistry.cas.org/detail?cas_rn=123154-38-1 | |
| Description | CAS Common Chemistry is an open community resource for accessing chemical information. Nearly 500,000 chemical substances from CAS REGISTRY cover areas of community interest, including common and frequently regulated chemicals, and those relevant to high school and undergraduate chemistry classes. This chemical information, curated by our expert scientists, is provided in alignment with our mission as a division of the American Chemical Society. | |
| Explanation | The data from CAS Common Chemistry is provided under a CC-BY-NC 4.0 license, unless otherwise stated. | |
| Record name | Tramadol | |
| Source | CAS Common Chemistry | |
| URL | https://commonchemistry.cas.org/detail?cas_rn=27203-92-5 | |
| Description | CAS Common Chemistry is an open community resource for accessing chemical information. Nearly 500,000 chemical substances from CAS REGISTRY cover areas of community interest, including common and frequently regulated chemicals, and those relevant to high school and undergraduate chemistry classes. This chemical information, curated by our expert scientists, is provided in alignment with our mission as a division of the American Chemical Society. | |
| Explanation | The data from CAS Common Chemistry is provided under a CC-BY-NC 4.0 license, unless otherwise stated. | |
| Record name | Tramadol [INN:BAN] | |
| Source | ChemIDplus | |
| URL | https://pubchem.ncbi.nlm.nih.gov/substance/?source=chemidplus&sourceid=0027203925 | |
| Description | ChemIDplus is a free, web search system that provides access to the structure and nomenclature authority files used for the identification of chemical substances cited in National Library of Medicine (NLM) databases, including the TOXNET system. | |
| Record name | (+)-trans-Tramadol free base | |
| Source | ChemIDplus | |
| URL | https://pubchem.ncbi.nlm.nih.gov/substance/?source=chemidplus&sourceid=0123154381 | |
| Description | ChemIDplus is a free, web search system that provides access to the structure and nomenclature authority files used for the identification of chemical substances cited in National Library of Medicine (NLM) databases, including the TOXNET system. | |
| Record name | Tramadol | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00193 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Tramadol | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID90858931 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
| Record name | (1R,2R)-2-[(Dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexanol | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID401167150 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
| Record name | Tramadol | |
| Source | European Chemicals Agency (ECHA) | |
| URL | https://echa.europa.eu/substance-information/-/substanceinfo/100.043.912 | |
| Description | The European Chemicals Agency (ECHA) is an agency of the European Union which is the driving force among regulatory authorities in implementing the EU's groundbreaking chemicals legislation for the benefit of human health and the environment as well as for innovation and competitiveness. | |
| Explanation | Use of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page. | |
| Record name | TRAMADOL | |
| Source | FDA Global Substance Registration System (GSRS) | |
| URL | https://gsrs.ncats.nih.gov/ginas/app/beta/substances/39J1LGJ30J | |
| Description | The FDA Global Substance Registration System (GSRS) enables the efficient and accurate exchange of information on what substances are in regulated products. Instead of relying on names, which vary across regulatory domains, countries, and regions, the GSRS knowledge base makes it possible for substances to be defined by standardized, scientific descriptions. | |
| Explanation | Unless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required. | |
| Record name | TRAMADOL, (+)- | |
| Source | FDA Global Substance Registration System (GSRS) | |
| URL | https://gsrs.ncats.nih.gov/ginas/app/beta/substances/0NG5TTM63P | |
| Description | The FDA Global Substance Registration System (GSRS) enables the efficient and accurate exchange of information on what substances are in regulated products. Instead of relying on names, which vary across regulatory domains, countries, and regions, the GSRS knowledge base makes it possible for substances to be defined by standardized, scientific descriptions. | |
| Explanation | Unless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required. | |
| Record name | TRAMADOL | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/7047 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
| Record name | Tramadol | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0014339 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Melting Point |
178-181 °C, 180 - 181 °C | |
| Record name | Tramadol | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00193 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Tramadol | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0014339 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
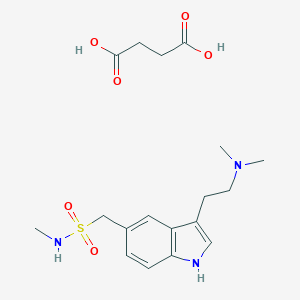
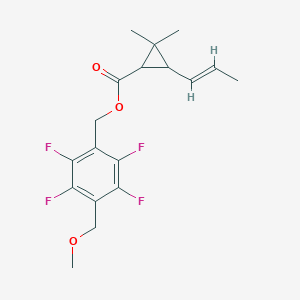
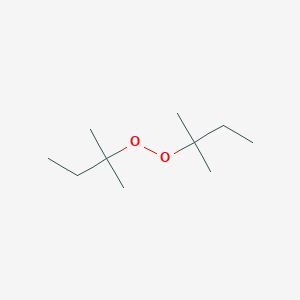
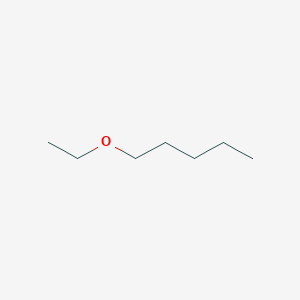
Synthesis routes and methods I
Procedure details





Synthesis routes and methods II
Procedure details





Synthesis routes and methods III
Procedure details




Retrosynthesis Analysis
AI-Powered Synthesis Planning: Our tool employs the Template_relevance Pistachio, Template_relevance Bkms_metabolic, Template_relevance Pistachio_ringbreaker, Template_relevance Reaxys, Template_relevance Reaxys_biocatalysis model, leveraging a vast database of chemical reactions to predict feasible synthetic routes.
One-Step Synthesis Focus: Specifically designed for one-step synthesis, it provides concise and direct routes for your target compounds, streamlining the synthesis process.
Accurate Predictions: Utilizing the extensive PISTACHIO, BKMS_METABOLIC, PISTACHIO_RINGBREAKER, REAXYS, REAXYS_BIOCATALYSIS database, our tool offers high-accuracy predictions, reflecting the latest in chemical research and data.
Strategy Settings
| Precursor scoring | Relevance Heuristic |
|---|---|
| Min. plausibility | 0.01 |
| Model | Template_relevance |
| Template Set | Pistachio/Bkms_metabolic/Pistachio_ringbreaker/Reaxys/Reaxys_biocatalysis |
| Top-N result to add to graph | 6 |
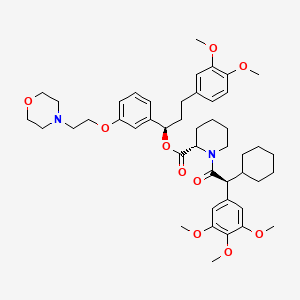
Feasible Synthetic Routes
Disclaimer and Information on In-Vitro Research Products
Please be aware that all articles and product information presented on BenchChem are intended solely for informational purposes. The products available for purchase on BenchChem are specifically designed for in-vitro studies, which are conducted outside of living organisms. In-vitro studies, derived from the Latin term "in glass," involve experiments performed in controlled laboratory settings using cells or tissues. It is important to note that these products are not categorized as medicines or drugs, and they have not received approval from the FDA for the prevention, treatment, or cure of any medical condition, ailment, or disease. We must emphasize that any form of bodily introduction of these products into humans or animals is strictly prohibited by law. It is essential to adhere to these guidelines to ensure compliance with legal and ethical standards in research and experimentation.